Adverse drug reactions

Adverse drug reactions
Table of Contents
Definition of Adverse drug reaction
Adverse drug reactions (ADR’s) are an important clinical problem.
According to a World Health Organization (WHO), an ADR has been defined as
“A response to a drug which is noxious and unintended, and which occurs at doses normally used in man for the prophylaxis, diagnosis, or therapy of disease, or for the modification of physiological function”.
Thus, this definition excludes therapeutic failures, overdoes (either accidental or intentional), drug abuse, non-compliance, and medication errors.
The terms adverse drug reaction and adverse event (AE) are not synonymous.
According to WHO, Adverse Event is defined as “Any untoward medical occurrence in a patient or clinical investigation subject administered a pharmaceutical product and which does not necessarily have to have a causal relationship with this treatment.
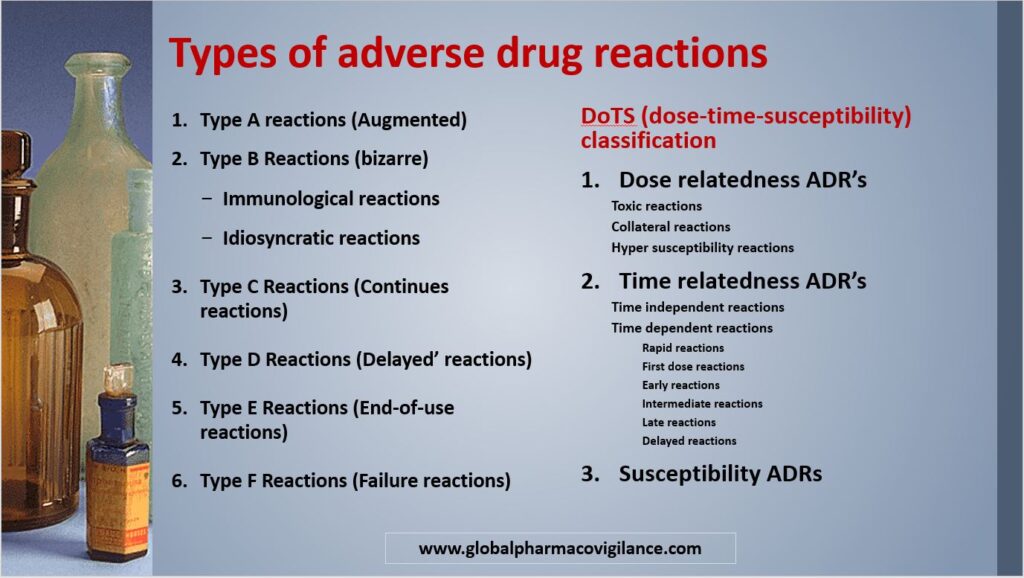
Types of adverse drug reactions
History of Types of adverse drug reactions
| Year | Action |
| 1977 | Adverse drug reactions were classified into Type A and Type B reactions |
| 1981 | Type A and Type B reactions were assigned with mnemonic labels i.e., augmented and bizarre respectively |
| 1984 | Subsequently, two further types of reaction were added: reactions related to both dose and time, and delayed reactions and 1992-labelled as types C and D |
| 1992 | Splits type C into two types, type C (continuous) and type E (end of use) |
| 2000 | Adds a sixth category, F for failure |
| 2002 | Adds a seventh category, G for genetic/genomic |
| 2003 | DoTS-distinguishes three types of dose-related reactions—toxic, collateral, and hypersusceptibility reactions |
Rawlins and Thompson have classified adverse drug reactions into type A and type B on the basis of the dose and mechanism of action.
Type A reactions (Augmented)
- Type A reactions are consistent with an increase in a drug’s pharmacological actions. Therefore, these are also called pharmacological adverse reactions
- They are dose-dependent and thus easily reversible when reducing the dose or withdrawing the medication.
- Type A adverse drug reactions occur more frequently than Type B reactions, accounting for more than 80% of all reactions
- Type A reactions morbidity was high and mortality was low
- Type A reactions are pharmacologically predictable
- Type A reactions are generally less severe
- They are usually detected in clinical trials performed before commercialization.
Type A reactions Examples
Toxic effects
Digoxin toxicity, serotonin syndrome with Selective serotonin reuptake inhibitors (SSRIs)
Side effects
Anticholinergic actions of tricyclic antidepressants causing tachycardia, dryness of the mouth, and blurring of vision
Factors that affected the pharmacological adverse reactions include
- Dose
- Pharmaceutical variation in drug formulation
- Pharmacokinetic abnormalities
- Pharmacodynamic abnormalities
- Drug-Drug interactions
Pharmaceutical
Differences in the pharmaceutical formulation can give rise to substantial alterations in the quantity of the drug that is “available” to reach its site of action
Pharmacokinetic
- Individual differences in absorption, distribution, and elimination result in differences in drug concentrations at the site of action.
- Enhanced absorption, or impaired elimination, cause an increase in plasma and tissue concentrations and may precipitate type A toxicity.
- Conversely, reduced absorption or accelerated elimination can cause therapeutic failure.
- Pharmacokinetic variability is therefore an important and common cause of type A reactions.
- The most common pharmacokinetic cause for type A reactions is variability in the rate of elimination.
- The elimination of drugs excreted unchanged by the kidney is directly proportional to renal function.
Pharmacodynamic
- Although pharmacokinetic variability is significant, at least some of the individual drug sensitivity is due to altered target organ sensitivity.
- Although this has been insufficiently studied, changes in receptors (density and affinity) and alterations in homeostatic mechanisms are likely to be affected.
- Altered target organ response accounts for much of the variation in response to warfarin and for the rare condition of hereditary resistance.
| Factors | Pharmaceutical | Pharmacokinetic | Pharmacodynamic |
| Drugs | Osmosin (slow-release indomethacin) | Digoxin | Indomethacin |
| Mechanism | Release of high concentrations of active
drug locally in gastrointestinal tract |
Decreased elimination if renal function is
impaired |
Water and sodium retention |
| Outcome-Type A reactions | Gastrointestinal bleeding | Nausea, vomiting, arrhythmias | Left ventricular failure |
Type B Reactions (bizarre)
- Type B adverse events are unusual (bizarre) and cannot be predicted based on the known pharmacology of the drug. Therefore, they are called pharmacologically unexpected or idiosyncratic adverse reactions.
- They are dose-independent and unpredictable and affect only predisposed individuals.
- Type B responses are less frequent but often severe and are responsible for many deaths.
- The morbidity of type B reactions was low, with high mortality.
Type B Reactions are subdivided into
Immunological reactions
Hypersensitivity involving one or several immunologic mechanisms. E.g., Penicillin hypersensitivity
Idiosyncratic reactions
Non-immunological hypersensitivity is not explainable by the pharmacological properties of a drug. E.g., Acute porphyria Malignant hyperthermia Pseudo allergy (e.g., Ampicillin rash)
Factors that affected the Type B reactions include
- Pharmaceutical
- Pharmacokinetic
- Pharmacodynamic
Pharmaceutical
- By-products of chemical synthesis – for instance, aspiryl anhydride, -or in-vitro degradation products, such as tetracyclines and penicillins, may give rise to toxic effects that have no relation to a drug’s known pharmacological properties.
- Similarly, the additives, excipients, colorisers, and binders that make up a pharmaceutical product-for example, lactose, glutein, tartrazine-may themselves cause toxicity or may react with the drug itself to yield toxic derivatives such as carboxymethylcellulose and penicillin.
Pharmacokinetic
- Individual differences in the overall rate and extent of absorption, distribution, and elimination results in changes in the intensity of a drug’s effects.
- It is theoretically possible, however, that the toxicity of some compounds is mediated via the formation of unusual, or novel, metabolites.
- There is evidence that the hepatotoxicity of methyldopa and isoniazid may be due to this process.
- It has also been suggested that the formation of electrophilic drug metabolites, which can bind covalently to tissue macromolecules, may result in the production of complete antigens or autoantibodies, but at present, there is no convincing example of such a mechanism at work.
Pharmacodynamic
Some type B reactions are due to genetic abnormalities that result in altered target organ responses.
These include
- Hemolysis with oxidant drugs-for instance, sulphonamides, 8-aminoquinolines in individuals with red cell glucose-6-phosphate dehydrogenase deficiency or certain haemoglobinopathies
- The precipitation of acute porphyria with enzyme inducing agents
- Malignant hyperpyrexia with inhalational anaesthetics and muscle relaxants
- Periodic paralysis with drugs that alter some potassium
Classification (Type A and Type B) is simple. It assists with drug regulation, as pre-licensing studies may reveal Type A reactions, and predicts that dose titration will reduce the risk of certain reactions.
However, it is sometimes difficult or not possible to assign a response to a type.
For instance, Dose dependent (type A) – Nausea and vomiting associated with erythromycin can also be categorized as Type B because they are not pharmacologically predictable.
In addition, the system does not easily classify other types of adverse reactions.
For instance, Osteoporosis of corticosteroids depends not only on the dosage but also on the length of treatment. And certain reactions, like asthma from ß-adrenoceptor antagonists, do not occur in all patients.
Further categories of ADRs were subsequently proposed where Type A and Type B were found to be insufficient to classify ADRs.
Type C Reactions (Continues reactions)
- The reactions are dose- and time-dependent.
- These reactions result from long-term (chronic) drug use.
- These are related to duration and dosage of exposure.
- These are uncommon reactions
- These reactions are managed by reduce dose or withhold and withdrawal may have to be prolonged
Examples:
- Hypothalamic pituitary adrenal suppression from glucocorticoid therapy
- osteonecrosis of the jaw with bisphosphonates
Type D Reactions (Delayed’ reactions)
- These reactions are Time-related.
- Type D Reactions are the reactions that become apparent sometime after the use of a drug treatment. The timing of these may make them more difficult to detect.
- Type D Reactions are uncommon
Examples:
- Leucopoenia-which can occur up to six weeks after a dose of lomustine
- Tardive dyskinesia with neuroleptics
Type E Reactions (End-of-use reactions)
- These reactions are associated with the withdrawal of the drug.
- Type E Reactions are uncommon
- These reactions are managed by reintroduce and slowly withdrawal of drug
Examples: Insomnia, anxiety and perceptual disturbances following the withdrawal of benzodiazepines and myocardial ischaemia caused by β-blocker withdrawal.
Type F Reactions (Failure reactions)
- Type F Reactions are due to unexpected failure of therapy
- Type F Reactions are common and Dose-related
- These reactions may be caused by drug interactions
- These reactions are managed by increasing the dosage of drug and by concomitant therapy.
Example: Failure of oral contraceptives due to induction of enzymes by a second drug
DoTS (dose-time-susceptibility) classification
The A/B classification is defined only by properties of the drug-its known pharmacology and the dose dependence of its effects.
However, other criteria should be taken into account in a comprehensive classification, including
- Properties of the reaction (the time course of its appearance and its intensity)
- Properties of the individual (the genetic, pathological, and other biological differences that confer susceptibility).
In 2003, Aronson and Ferner proposed a three-dimensional classification system based on dose relatedness, timing, and patient susceptibility (DoTS).
Dose relatedness Adverse drug reactions
There are three classes of dose-related adverse drug reactions, which are categorized according to the concentration at which they occur in relation to the therapeutic concentration in an individual, as follows:
Toxic reactions
Adverse drug reactions occurs at supratherapeutic concentrations
Example: syncope due to a nitrate is a toxic reaction
Collateral reactions
Adverse drug reactions occur at standard therapeutic concentrations.
Example: Osteoporosis due to corticosteroids
Hyper susceptibility reactions
Adverse drug reactions occurs at sub-therapeutic doses in susceptible patients
Example: Anaphylaxis due to penicillin
Time relatedness Adverse drug reactions
There are two categories of time relatedness of adverse drug reactions time-independent and time-dependent.
Time independent reactions
Time-independent reactions occur at any point during treatment, regardless of course length. They typically occur either when
- the amount of drug being administered changes by a pharmaceutical mechanism e.g., altered availability from a pharmaceutical formulation
- the concentration of the drug at the site of action changes by a pharmacokinetic mechanism e.g., digoxin toxicity when renal function worsens
- the pharmacological response is altered by a pharmacodynamic mechanism without a change in concentration at the site of action e.g., digoxin toxicity in association with potassium depletion
When such a reaction occurs, its duration may be affected by the kinetics of the medication, but it is not an aspect of its time dependence as defined here.
Time-dependent reactions
There are six subtypes of time-dependent reactions – rapid, first dose, early, intermediate, late, and delayed.
Rapid reactions
Rapid reactions only happen when a medication is administered too quickly. e.g., the red man syndrome with vancomycin
First dose reactions
Reactions to the first dose occur after the first dose and not necessarily afterwards. e.g., hypotension after the first dose of an angiotensin-converting enzyme inhibitor and type I hypersensitivity reactions
Early reactions
Early reactions occur early in treatment and then diminish with ongoing treatment. These are adverse drug reactions to which patients develop tolerance (such as nitrate induced headache).
Intermediate reactions
- Intermediate reactions occur after some delay; however, if a reaction has not occurred after a certain time, there is little or no risk that it will occur later.
- E.g., Hypersensitivity reactions of type II (thrombocytopenia due to quinine), type III (interstitial nephritis with penicillins), and type IV (cutaneous hypersensitivity to antihistamines), and the ampicillin/amoxicillin pseudoallergic rash. Non-allergic reactions of this type include the increased risk of neutropenia with carbimazole and of venous thromboembolism with antipsychotic drugs.
- Intermediate reactions occur in different susceptible populations.
- Those at high risk have the reaction and stop taking the drug; those at low risk do not have the reaction and can be regarded as healthy survivors. Thus, after a time the population risk seems to fall.
Late reactions
Late reactions occur rarely or not at all at the beginning of treatment, but the risk increases with continued or repeated exposure.
E.g., Many of the adverse effects of corticosteroids and tardive dyskinesia with dopamine receptor antagonists.
Withdrawal reactions are late reactions that occur when a drug is withdrawn or its dose is reduced after prolonged treatment.
E.g., Opiate and benzodiazepine withdrawal syndromes, hypertension after withdrawal of clonidine or methyldopa, and acute myocardial infarction after withdrawal of β blockers.
Delayed reactions
Delayed reactions are observed sometime after exposure, even if the drug is withdrawn before the reaction appears.
E.g., Carcinogenesis (vaginal adenocarcinoma in women who were exposed to diethylstilbestrol in utero) and teratogenesis (phocomelia due to thalidomide).
Susceptibility
- The risk of adverse effects varies according to the members of the exposed population.
- In some cases, the risk of adverse effects will be present in sensitive individuals and absent in others.
- In other cases, susceptibility follows a continuously distributed pattern.
E.g., Increasing susceptibility with increasing impairment of renal function
- While the causes of hypersusceptibility may be unknown, several types are recognized. These include genetic variation, age, sex, physiological variation, exogenous factors, and disease.
More than one susceptibility factor may occur.
Examples of DoTS (dose-time-susceptibility) classification
| ADR’s | Dose | Time | Susceptibility |
| Osteoporosis due to corticosteroids | Collateral effect | Late | age, sex |
| Anaphylaxis due to penicillin | Hypersusceptilbility | First dose | not understood-requires previous sensitisation |
| Hepatotoxicity due to isoniazid
|
Collateral effect | Intermediate | genetic (drug metabolism), age, exogenous (alcohol), disease (malnutrition) |
References:
- Edwards IR, Aronson JK. Adverse drug reactions: definitions, diagnosis, and management. Lancet. 2000 Oct 7;356(9237):1255-9.
- Meyboom RH, Lindquist M, Egberts AC. An ABC of drug-related problems. Drug Saf. 2000 Jun;22(6):415-23.
- Rawlins MD, Thompson JW. Pathogenesis of adverse drug reactions. In; Davies DM, ed. Textbook of adverse drug reactions. Oxford: Oxford University Press, 1977: 10.
- Rawlins MD, Thompson JW. Pathogenesis of adverse drug reactions. In: Davies DM, ed. Textbook of adverse drug reactions, 2nd edn. Oxford: Oxford University Press, 1981: 11.
- Grahame-Smith DG, Aronson JK. Adverse drug reactions. In: The Oxford textbook of clinical pharmacology and drug therapy. Oxford: Oxford University Press, 1984: 132–57.
- Royer RJ. Mechanism of action of adverse drug reactions: an overview. Pharmacoepidemiol Drug Saf 1997; 6 (Suppl 3): S43–50.
- Hartigan-Go KY, Wong JQ. Inclusion of therapeutic failures as adverse drug reactions. In: Aronson JK, ed. Side effects of drugs, annual 23. A worldwide yearly survey of new data and trends in adverse drug reactions. Amsterdam: Elsevier (in press).
- Patrick Waller. An introduction to pharmacovigilance. John Wiley & Sons, 2007
- Johannes Ring and Knut Brockow. Adverse Drug Reactions: Mechanisms and Assessment. Eur Surg Res 2002;34:170–175
- Munir Pirmohamed, Alasdair M Breckenridge, Neil R Kitteringham, B Kevin Park. Fortnightly review: Adverse drug reactions. BMJ. 1998 Apr 25; 316(7140): 1295–1298.
- Aronson JK, Ferner RE. Joining the DoTS: new approach to classifying adverse drug reactions. BMJ. 2003 Nov 22;327(7425):1222-5.
- Rawlins MD. Clinical Pharmacology: Adverse Reactions To Drugs. BMJ. 1981 Mar 21; 282(6268): 974-976.
- Khraenbuhl-Melcher A, Schlienger R, Lampert M, et al. Drug – related problems in hospitals. A review of the recent literature. Drug Safety 2007; 30: 379-407.
- Word Health Organization. International drug monitoring: the role of the hospital. Geneva, Switzerland: word health organization;1966. technical report series no.425.
What is the Pharmacovigilance process?
I agree with you